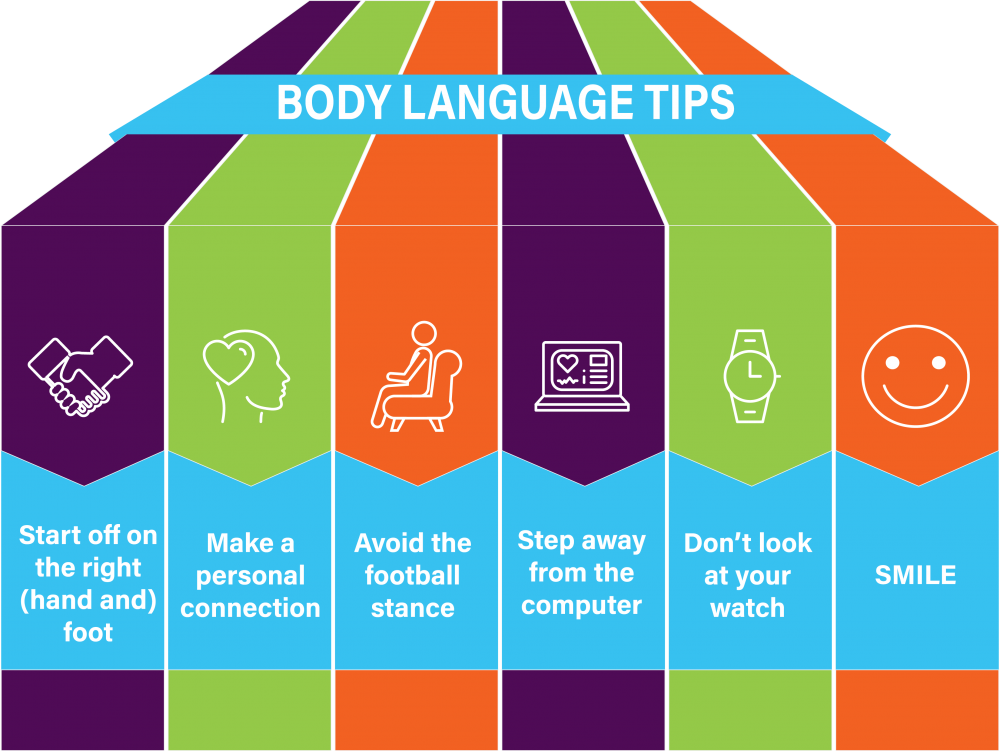
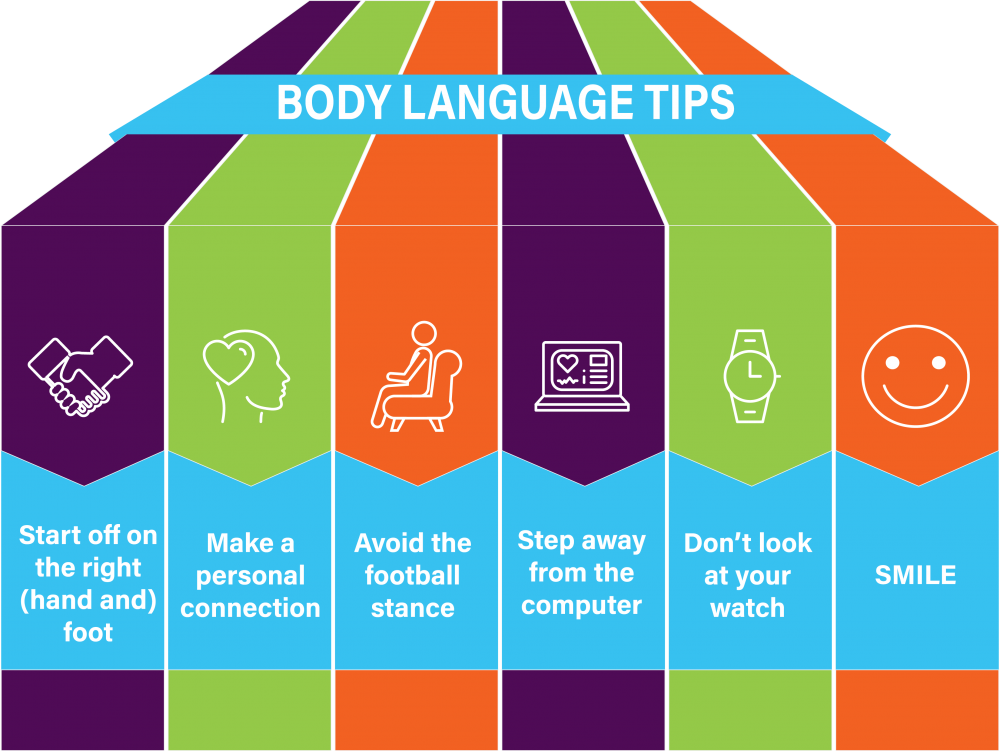
When you think about improving your patient experience scores, you might be quick to focus on your office décor or new equipment without pausing to think about the little things that can add up to a big deal in the minds of a patient. An interaction that garners high patient experience scores may be much easier than you thought. Displaying positive body language can help you make better connections, earn stronger reviews, and enjoy better long-term relationships with your patients. Try one of these tips to get underway:
- Start off on the right (hand and) foot. When you introduce yourself to a patient or caregiver, do so with a handshake or gentle touch, maintaining eye contact and focus on the other person. Apologize, even if the patient has only been waiting a few minutes with the recognition that, “I know your time is valuable, and I am sorry I kept you waiting.”
- Make a personal connection. When you initiate a conversation with a patient, try to start the conversation with a personal detail – perhaps you recall something from the patient’s last visit, such as an upcoming vacation, or you can offer a nice compliment or even a relevant comment about the weather. Don’t linger, since it is important to start the visit, however, this brief moment that serves to establish or foster a personal relationship can be incredibly meaningful to the patient and ease discomfort over the visit itself.
- Avoid the football stance. Even when football season is long over, too many physicians have an ingrained habit of sitting down with knees open and back arched, with their hands on hips or arms crossed. This creates a defensive posture that doesn’t invite much confidence or trust. Keep your arms open, your chest lifted, and your posture welcoming. Lean in, not out.
- Step away from the computer. When you get attached to a keyboard or a tablet, it is easy to follow it with your eyes, rather than making that connection with your patient. Turn off your screen and listen to your patient’s concerns before launching into anything else.
- Don’t look at your watch. While we all know that time is of the essence, patients tend to feel rushed when they see a physician looking at his or her watch. To keep better track of time, you can install clocks above the “heads” of exam room tables, or you can check your watch before entering the room.
- Smile. Even if the visit is covering serious information, a welcoming smile or a reassuring glance can make your patients feel that much more comfortable. In addition, eye contact is critical – no matter what information you are conveying.
Ultimately, your body language with patients may be just as important as the information you discuss and the plans you make. In order to care for your patients, your patients must perceive that you care about them. Most often, we are not aware of our body language, so try to understand yours – and take strides to improve it. Body language can make the difference between comfort and discomfort, good ratings and bad, a one-time visit and a long-term connection. If these “soft” skills don’t come naturally to you, practice making eye contact, keeping your posture and the lines of communication open so that you invite greater trust and ease with each patient you meet.
The contents of The Sentinel are intended for educational/informational purposes only and do not constitute legal advice. Policyholders are urged to consult with their personal attorney for legal advice, as specific legal requirements may vary from state to state and/or change over time.