Readers of this article may be familiar with the medication error case that resulted in a fatality at Vanderbilt University Medical Center back in 2017. That medication error involved a nurse who gave the patient vecuronium, a muscle paralytic instead of Versed, a sedative, which resulted in the death of a patient. Not only was Vanderbilt sued in civil court by the family of the patient, but the nurse was convicted of criminally negligent homicide due to the death of the patient. While most medication errors do not result in death, the following story should serve as a reminder that medical providers and administrators should implement, consistently follow, and continuously review medication protocols to ensure patient safety and to avoid negative outcomes.
Mary White,[1] was 28 years of age and at the end of a full-term pregnancy. She presented to the hospital’s labor and delivery department for a planned induction of labor and was also scheduled for a post-partum tubal ligation. The anesthesia team on duty consisted of Buddy Michaels, M.D. and Terry Lawler, CRNA.
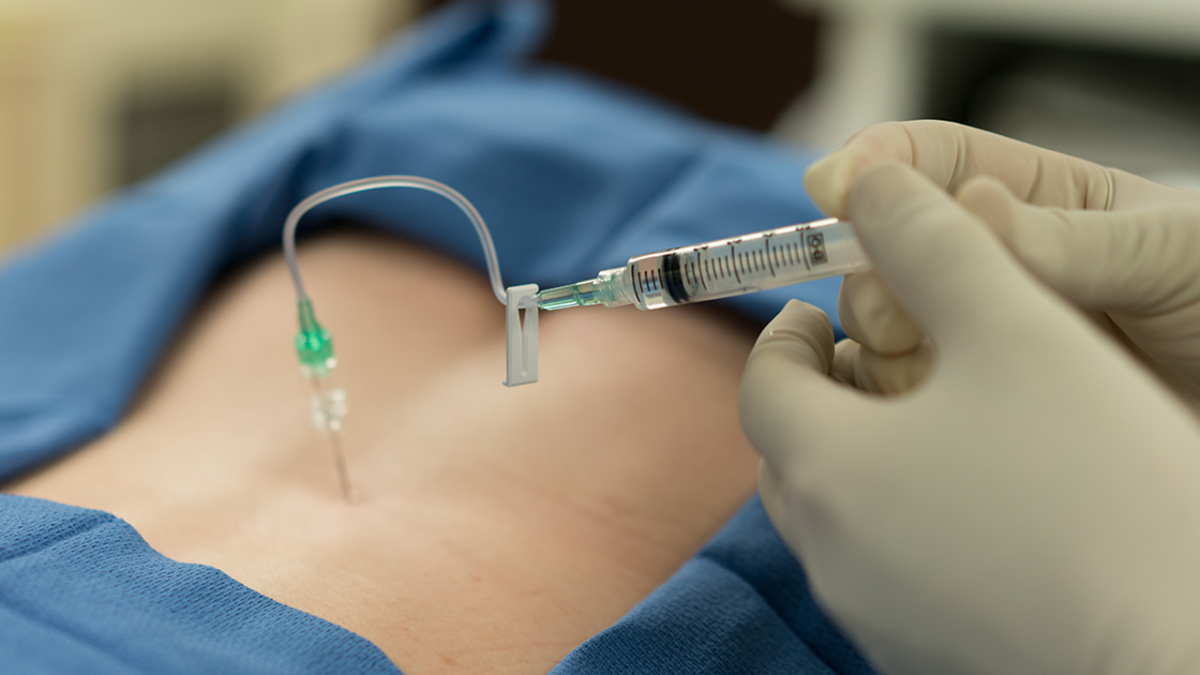
CRNA Lawler was responsible for placing the epidural catheter and administering the obstetric anesthesia. The baby was delivered without any complications. After the delivery, and in anticipation of the tubal ligation, CRNA Lawler injected the patient’s epidural catheter with two medications. The medications to be given were midazolam (Versed) and ondansetron (Zofran), to prevent nausea. When CRNA Lawler began to push what was believed to be Versed through the I.V., the patient complained that her I.V. site was burning and asked for it to be stopped. Mrs. White soon complained of a severe headache and generally feeling bad. She began to vomit and then lost consciousness. CRNA Lawler immediately called for Dr. Michaels who quickly responded to assess the situation. A nurse noted that the patient’s blood pressure was elevated, and her heart rate was low. Auscultation revealed an irregular heart rhythm.
Time was of the essence given the patient’s deteriorating condition. Believing that the patient had experienced an allergic reaction to the anesthesia, the patient was given a reversal agent for the Versed. Dr. Michaels requested an immediate EKG and a cardiology consult. A CT scan of the brain was obtained as the patient continued to complain of a persistent headache. Due to the quick intervention, her vital signs eventually stabilized. Mrs. White continued to complain of a headache and not feeling well. Her troponin level was elevated, and a telemetry strip showed a sinus rhythm with sinus bradycardia. After her discharge, it was necessary for Mrs. White to continue seeing a cardiologist for monitoring to be sure she did not sustain any permanent cardiac injuries.
After this incident, the anesthesia team reflected upon the process of how the medication was delivered to the floor for its use in this case and came to the realization that the patient was most likely given a large dose of phenylephrine, a vasoconstrictor that increases blood pressure, when she was supposed to be given Zofran. The method in which the medication was delivered to the labor and delivery floor from the pharmacy aided in the confusion. Two separate medication boxes were provided to CRNA Lawler. One box contained anesthetic medications. The second box contained medications required for labor and delivery. The Zofran was placed near the phenylephrine. Notably, both vials were of similar size, and the color of the caps were the same. In a high pressure and fast-paced environment like labor and delivery, the medications should not have been presented in this manner. Placing the different medications right next to each other was the recipe for a medical emergency.
A lawsuit was filed on behalf of Mrs. White alleging that the negligent administration of phenylephrine caused the cardiac event resulting in permanent physical, mental, and emotional injuries. In addition to Dr. Michaels and CRNA Lawler being sued, the hospital was named in the suit alleging failure to properly store the vials of medication in an appropriate location and manner. More specifically, the suit alleged that it was a deviation from the standard of care to present medications that were not easily distinguishable from each other in such close proximity.
Part of Plaintiff’s theory of negligence in the case was focused on how the drugs were administered. Another theory focused on how the medications were obtained from the pharmacy, as there was no notation made in the chart regarding whether the drugs were stored near the operating room in an automated dispensing cabinet or if the drugs were delivered to the operating room from the pharmacy. A key takeaway here is that plaintiffs’ counsel often tends to exploit what is not noted in the chart and then make the omission a key element of its case. Medical record documentation is an issue in many medical malpractice cases. Appropriate charting should always be a priority.
The defense of the case was developed through written discovery, the retention of expert witnesses, and depositions. It became clear that Dr. Michaels was not involved in the physical selection or administration of the medications that led to this incident. Eventually, he was dismissed from the case. Further, the defense was able to develop evidence that the patient did not suffer long-term cardiac damage due to this unfortunate event.
The proximity of the medications being placed in similar looking containers does not excuse the fact that the incorrect type of medicine was given to the patient. Yet, better protocols in this situation likely would have produced a more favorable outcome. In hindsight, which is the way most of these stories are told, this unfortunate event could have been avoided if only a few safeguards had been in place in the labor and delivery department on that day.
Whether you practice in a hospital or office setting, consider the tips below to avoid medication errors.
With a defense in place regarding the lack of permanent damages, the parties agreed to submit the matter to a mediator for settlement negotiations. Thereafter, the case settled without the necessity of a trial.
For more information on this topic see “Safe Medication Practices in the Physician Office”[2] by Julie Loomis, R.N., J.D., Assistant Vice President of Risk Education.
[1] Names and identifying details have been changed for confidentiality.
[2] Safe Medication Practices in the Physician Office by Julie Loomis, RN, JD - https://www.svmic.com/resources/newsletters/119/safe-medication-practices-in-the-physician-office
The contents of The Sentinel are intended for educational/informational purposes only and do not constitute legal advice. Policyholders are urged to consult with their personal attorney for legal advice, as specific legal requirements may vary from state to state and/or change over time.