Dr. Dike Drummond of The Happy MD speaks with Brian Fortenberry about physician burnout. Understanding burnout is not that simple, and Dr. Drummond helps doctors navigate circumstances that can lead to this state. He shares some practical tips on prevention and how to get out of the rut.
Speaker 1: You're listening to Your Practice Made Perfect: Support, Protection and Advice for Practicing Medical Professionals. Brought to you by SVMIC.
Brian: Hello, welcome to our episode of this week's podcast. We're going to be talking about a topic today of great interest to many, not only in healthcare, but really in any area of life in our busy society. Today, we're going to be talking about burnout. My name is Brian Fortenberry. Joining me today is Dr. Dike Drummond. Dr. Drummond, thanks for being here.
Dr. Drummond: My pleasure.
Brian: Well, and this is an exciting thing for us. This is going to be almost like a little preview of some stuff you're going to be doing for us on the live seminars for SVMIC. You're going to be getting more in depth in this topic of burnout, but really today we just kind of want to get a brief introduction to the topic and get folks excited about what's to come in the seminars coming up in 2019. Why don't you start by telling us a little bit about yourself, about your background, your professional and personal information Dr. Drummond?
Dr. Drummond: Well, I went to medical school in Rochester, Minnesota at Mayo. Mayo's got a tiny little medical school in their campus.
Brian: Very small.
Dr. Drummond: Very small, 40 in each year but the resident campus has got 5000 residents. So, I spent my four years in Minnesota and then went to California to do my family practice residency in Reading which recently burned in the car fire. Then moved to Mount Vernon in Washington, which is halfway between Seattle and Vancouver B.C. and set up my practice and raised my family there, and for 10 years I was a full spectrum family doc. In 1999, I burned out of my practice in a fantastic fashion that you'll learn about if you come to the live seminar, and eventually had a very successful little training company teaching people how to lead better meetings, meeting facilitation and leadership development the Navy's Lean Six Sigma Black Belt certification program, interestingly enough. In 2010, I launched The Happy MD as a coach to be able to help doctors who were feeling burned out like I did back in 1999.
For the last seven years, we've been the leading organization to provide coaching and training and consulting to prevent physician burnout both for individual doctors and for organizations. At this point in time, I have trained about 30,000 doctors for 140 organizations in three different continents. I'm happy to be able to come and work with SVMIC to bring these principles to the folks that are your subscribers.
Brian: Well, we really appreciate it because this is certainly a topic that I know we all face at some point, but it seems to really be something that is being talked about these days. You said you experienced burnout yourself?
Dr. Drummond: Absolutely.
Brian: What kind of got you there in a brief synopsis that you were able to pinpoint that, "Oh, wow, here I am and how did I get here and now what am I going to do about it?"
Dr. Drummond: The challenge is I didn't realize what had happened to me until years later. That's one of the challenges of burnout, is the person who's overstressed and suffering from it, usually doubles down and works even harder. That's what we learned to do in our residency program, because residency is about survival. It's often that the doctor is the last person to recognize they have burnout. It actually took me three or four years to figure out that burnout is what had taken me out. In my case, my family had wanted to have a doctor in the family for three generations and I was the one who fulfilled that dream for them.
Brian: Sure.
Dr. Drummond: But at that point in time, the two people who wanted it the most when I was 40, my mom and my grandma were both dead. I had been a family doc for 10 years and I just hit a brick wall. For me it felt like somebody was choking me out when I was at work. I took a sabbatical, it didn't get better, and I actually quit as a means of survival. Again, it's one of those things that I recommend people don't do is walk away from their current job no matter how bad they feel, because that's going to cut out some possibilities for you going forward. Don't do what I did; I learned some lessons the hard way. I'm going to teach you so that you don't have to repeat them.
Brian: Is that really what led you to create The Happy MD back in 2010?
Dr. Drummond: Well, I got certified as a coach right away and coaching is something that has a certification process; it's a different way of working with clients. But it was actually 10 years later, the second time I burned out, when a divorce in that business, the training business I talked about went away. It was in the depths of that, that I decided I would see if there was a way to help other doctors and that's when I launched The Happy MD.
It just happens that that was seven years ago, and the wave of interest in burnout has coincided with my website being number one on Google for physician burnout, if you type it in. We actually own about six positions on that first page, so at this point I have about 2300 hours of one-on-one physician coaching experience helping doctors from all specialties get better. Like I said, people have asked me if I can train and I've been pretty much full-time as a trainer, teaching doctors the lessons we've learned from their colleagues as coaches.
Brian: What are some of the reasons that you see physicians ending up in burnout? Can you put your finger on any of it?
Dr. Drummond: Oh, yeah.
Brian: Tell us a little about that?
Dr. Drummond: Absolutely, but it's not simple. See, the most difficult thing for doctors to do to understand burnout is realize it's not simple. It's not a problem, there isn't a solution. It's been a perfect storm of overload for the doctors in the front line. First of all, burnout is a combination of being totally exhausted, being cynical and sarcastic about your patients, and wondering whether or not your job or your practices having any meaningful impact at all. What's the use is a term that comes into your head. Typically, that's because of overwhelm. So, the most obvious things that's changed about medical practice in the last seven years is two main movements. Again, these aren't the causes of burnout, they're just some of the factors that add together for an individual doctor. One is obviously EMR, Electronic Medical Records.
Dr. Drummond: It used to be that you scribble on a chart and you'd be done. You didn't have to have a perfect storm of clicks and have to type 120 words a minute. Let's remember that it's not just EMR, its EMR and texts and patient portals and email all coming in all at once without you necessarily having additional staff to handle that load. The second big movement is that doctors who used to be independent are now often employees. It was 2017 that for the first time the majority of physicians were employees rather than independent. Now you work for the man and you got to fill out the EMR, that's not that dark, right?
Brian: No.
Dr. Drummond: However, boom, boom, all of a sudden being a doctor in 2018 is a lot different than being a doctor in 2010, and so I would say for most doctors, those two factors are major in their burnout. There's a lot more.
Brian: Do you see whenever you're dealing with these physicians, sometimes it probably could be misconstrued as I'm sitting here listening to you of you hear about doctors being, "Oh, we've got an issue. They're not playing well with others, they're not getting along with the staff or whatever." That could just be a symptom of burnout, correct?
Dr. Drummond: Yeah, if you're overwhelmed consistently and can't recharge at home. So, for instance, another big cause of burnout is whatever's going on at home. Because if you put energy into your practice and you come home and you're supposed to recover, but you can't recover at home because there's other things going on at home. Let's take a doctor who's on the edge coping with their practice just fine, but all of a sudden they have their first child and it turns out it's a special needs child. Or let's take any doctor and have their marriage start to fall apart or have them give them their own personal health issue. Now all of a sudden, your ability to recharge goes away, so you'll see people burn out beautifully at work, but it doesn't have anything to do with work either.
In any given case, the most important thing is that when you see somebody going down in flames, I call it a downward spiral, is to reach out and ask them how they're doing and see if you can figure out what's going on in that individual doctor. The challenge is, we've been conditioned to never show weakness, and so the chance that they'll tell you the truth the first time you reach out to them it's pretty slim. Again, one of the things I'll teach in the live session is how to reach out to a colleague in distress so that you have a better chance that they'll open up to you.
Brian: Obviously, there's going to be bleed over your personal life and professional life. Is it important to draw a very distinct line or is that really impossible?
Dr. Drummond: It's not impossible, but it's not something that's taught.
Brian: I got you.
Dr. Drummond: One of the things again that I'll teach is an off switch on your programming. I mean, basically, when you come home at night, you're still thinking about work, you're not recharging. Ideally, you would have an ability to flip a switch and turn the doctor off. When you're with a patient, hey, patient comes first. But the old saying, "I put your own mask on first”. At some point in time I have to let the patient go when I'm not with the patient, put myself first, because if you look at that little picture, it's always a picture of a woman putting her mask on with their child next to her. What happens if she doesn't put her mask on? They both die. It's life and death important that you find a way to recharge so that you can go back in again, and put the patient first when you're in front of them.
Brian: There's not a one size fits all when it comes to this?
Dr. Drummond: Never.
Brian: You hear people go, "Oh, well, here's the latest, greatest fix for this or the greatest fix for this or ...". And it's often not as simple as taking a pill, or it's not as simple as you do this, and there's myths out there that that can be the case. What are some of the myths that you have encountered when it comes to physician burnout?
Dr. Drummond: Well, and what you're talking about right now is the universal human urge for a magic potion, snake oil, cure all. What's the one thing? What do I need? What's the solution?
My answer is always, "I don't know, I need to ask you some questions to figure out what's causing your burnout in the first place." But, there's three myths that we'll bust in the live event. Number one, burnout doesn't have anything to do with your batteries being rundown. Number two, burnout's fundamentally not a problem, because it doesn't fit the definition criteria for the word problem. It doesn't have a solution, there's a different way that you address it. It's another S word, the word's actually strategy but I'll show you how that all fits together in the live event.
Those are the big three myths that I see. Actually, the simplest way that you can address burnout if you're an employee doctor, is there has to be a strategy for you and there has to be a strategy for the organization. Because, when a doctor is an employee of an organization, we got ourselves a canary in a coal mine situation there, so that both the canary and the coal mine need a strategy to lower the stress in the workplace.
Brian: There is a strategy obviously having to deal with physician burnout once you're there. Is there a different strategy to say prevent or try to keep at bay the possibility of physician burnout before you get there?
Dr. Drummond: Yeah, so let me give you a for instance. Somebody calls me on the phone at the website because they think they might want to coach, and our first session is always free. It's just a discussion of what's going on. We give people a strategic plan. They always want to tell me about what's going on, what's going wrong, what's not working for them on their job site. And they say, "what do you think I should do?" I always answer, "I have no idea, because it's one thing to know what's not working for you on your job site; it's a totally different thing to know what you'd like your practice to be." I always work with people to create an ideal job description and nobody teaches doctors to do that. But describe to me what you'd really like your practice to be like, because it's only when you know what that is that you can make the changes to get you there.
The first thing I always work with in coaches and the first thing we'll talk about in the training is how to create your own ideal job description, because you don't have to be burned out to benefit from the training here. No matter what is going on in your practice, this process of focusing on your ideal job will help you make it better. If you're 80% satisfied with your practice, we can get it to 85, 90 with the same process. But what I found is interesting, if you feel like you understand what your ideal practice is and you feel like you're moving in that direction, burnout just flat out doesn't happen.
Brian: Got you.
Dr. Drummond: As soon as you feel like you're swinging in the breeze and nobody cares, if that's what's going on, you can very easily get burned up. But as soon as you've identified what you want and you begin to move in that direction, all of that stress and burnout goes away because you're on a better path.
Brian: I think that's a perfect reason that people should understand, this is going to be seminars for everyone. You don't have to be in the heart of desperation of ‘I'm at my wits end’ and ‘it's the last straw, I'm burned out’. There's going to be information in this seminar that's going to be very beneficial for those people that haven't yet gotten to burn out.
Dr. Drummond: Right, and what's interesting too, is everywhere I go about 30% of the room's already been through it at least once.
Brian: Really?
Dr. Drummond: Because there is the highest and best use, right?
Brian: Yeah, so that is about 30% of any given group of physicians really.
Dr. Drummond: Here's burnout, okay? Remember back, I'm just talking to anybody who's listening right now, remember back to a time in your life, was there ever a time when you were being a good soldier doing what everybody expected of you, working hard, following orders, staying inside the lines and it got so uncomfortable that you had to make a change and that change is responsible for who you are today? Well, that discomfort at that turning point, that was burnout. It pushed you onto a path with more purpose, you're now happier now than you were back in that uncomfortable time.
See, the challenges though in that crisis point of ‘I can't take it anymore’, some people drink, drugs, end up statistics - suicide is even possible for burnout. We lose 400 doctors a year. So, what I help people do is actually use the stress and the burnout that they feel, to create that more ideal practice without having to go through the crisis that could take their life. Most rooms that I'm in about 30% of the doctors will raise their hand.
Brian: That is very interesting. It gets really real because in all of our lives, you often get to that, as you describe, that turning point and it's okay. Now, how am I going to deal with this?
Dr. Drummond: This isn't what I expected, right?
Brian: Right, exactly.
Dr. Drummond: I never thought it was going to be this way, but you look inside and at some point in time you say, "I've got to take responsibility, what am I going to do about it?" And you make the shift and it's like, "Why did I wait so long?"
Brian: Yeah, you're like, "Well, I had my life planned out. I was going to get married, I'm going to have the wife, two and a half children, the statistics say I was going to live with a white picket fence".
Dr. Drummond: Well, and check it out, though. If you're a doctor, residency and fellowship. I was a family doctor, four years of medical school, three years of residency; there's seven years in the medical education system. I've met people who've been as many as 20 years in medical education system. But that whole exercise is an exercise of survival. All I'm trying to do is make it to the end, realizing that they'll hold me underwater along the way.
Well, now I'm in my career, that career stretches to the horizon. This is a totally different setup. It's not just about survival, it's about, "Okay, now I'm out. It's my life." All of a sudden, I'm perhaps married, I perhaps have four children. Well, how is this going to work when now I'm on completely unfamiliar ground, because this isn't residency and it's not about survival and it won't be what you thought it was going to be, unless you're constantly planning to make it the best that you need it to be.
Brian: It has got to be extremely challenging to work with physicians that are becoming patients, I guess, to some extent in dealing with this burnout. How do you work with them? Is there a group that you have to pull in? How does that work?
Dr. Drummond: Well, as I said at my website, people contact me. So, the people that I work with are people who have woken up from the trance of just head down like little train on tracks. Most of the people that I work with are wanting to change and that's why it's so important to get out and do proactive education, because you don't have to wait till you're in a hole like that and ask for help from a position of burnout, to actually benefit from what we've learned from burnout doctors. But, no, I don't typically have to convince someone because what we teach is very, very, very simple stuff. Think about it, when I meet somebody, they're burned out. I cannot teach them things that are hard to understand and I can't ask them to try and do things that require a lot of time and energy. We have to take little baby steps that help them feel better right away, baby step, baby step, baby step.
It's little tiny changes and the most popular little tiny changes that my clients make for instant results are the six different tools that I teach in the live training. Like an off switch on your programming so you can come all the way home at night. Like a weekly process to create a life calendar, that only takes about 20 minutes every Sunday so that you can maintain life balance. Like understanding that you need a strategy and not a solution and beginning to build that. It's all very simple, we've burned out all the complicated stuff so everything I teach you will give you results immediately. The other thing that's interesting is having a group of doctors talk about the fact that this work is stressful and all of a struggle from time to time together, like we will in that room with the training. By itself is therapeutic. Because, you're going to realize you're not alone. Everybody feels this way. It's like, "Oh, you feel that way too?" It's just a relief to realize that you're not alone.
Brian: I think it's important for people to hear, sometimes you hear things and you're like, "They're going to give me this long list of stuff that I have to do that's going to take more of my time and be more complicated and it's just going to get me further down in the hole that I'm digging. This is not that, that is what I'm hearing.
Dr. Drummond: Right, if you have been to a burnout prevention training in the past, it probably sucked, because it was not something that was taught to you by a person who's coached 500 doctors and trained 20,000 more. I'm not going to tell you anything that's not real in the real world, because we've tested it with thousands of docs before it ever came out of my mouth. So that I'm not an academic, I'm not going to talk just about the topic, I'm going to give you tools. This is what it's like, here's a tool to prevent it. We're going to do that six times in the course of an hour and a half.
Brian: That's going to be an exciting time because this could really end up being life changing, life altering for physicians that one, either are in the depths of facing it or at least when you get to that turning point that we were talking about earlier, you can be prepared to know, "Okay, here's how I go."
Dr. Drummond: Don't wait for that.
Brian: Yeah.
Dr. Drummond: I'm going to teach people how to do date nights twice a month and you're going to call up your significant other and she or he is going to say, "What have you been smoking? Where have you been tonight? I shouldn't have let you out of the house today". I've had that happen all the time. Let's be real about what it takes to have the life that you want, if this isn't exactly it right now.
Brian: Well, as we get ready to wrap up this podcast and look forward to the live seminars, do you have any parting tidbits of information for people that might be listening right now? Maybe some things they can do if they're in desperation just at this very moment.
Dr. Drummond: Well, first of all, don't quit. Second of all, if you're hanging on by your toenails, what I would suggest is that you put the minimum amount of effort into your job that it takes to do a good job. Then, as you walk across the threshold of your home in the evening, take a great big breath and let all of that go, and then find someone. They may be in your call group or they may be a friend from residency. Find somebody that you can get real about how you're feeling, and hook up with that person as a support system to just talk about how you're feeling and begin to plan a way forward. You could always come to The Happy MD, it's thehappymd.com and get a free session with one of our coaches. We have six coaches that I've trained, they're all doctors, all certified coaches in the techniques that we use. But I would encourage you not to walk away and I would encourage you to open up to somebody, even if nobody reaches out to you. Open up to somebody and just tell them how you're really feeling and take it from there.
Brian: Could that somebody be really even in your house, like your spouse?
Dr. Drummond: Your spouse doesn't want to hear it anymore.
Brian: They're done with it, huh?
Dr. Drummond: You burn them out on your burnout. I would lean on someone else, either a colleague at your work site or a friend in healthcare who would understand what you're going through, a residency buddy, somebody in the local medical society, something like that would be my recommendation.
Brian: We can put information in the show notes links to your site and other information there. Thank you so much for being here today, having the opportunity to meet you and talk with you, and I would highly encourage anyone to join us in the seminars. Thanks for being here.
Dr. Drummond: Yeah, you're welcome.
Speaker 1: Thank you for listening to this episode of Your Practice Made Perfect with your host, Brian Fortenberry. Listen to more episodes, subscribe to the podcast, and find show notes at SVMIC.com/podcast. The contents of this podcast are intended for informational purposes only and do not constitute legal advice. Policyholders are urged to consult with their personal attorney for legal advice as specific legal requirements may vary from state to state and change over time.
The contents of this Podcast are intended for educational/informational purposes only and do not constitute legal advice. Policyholders are urged to consult with their personal attorney for legal advice, as specific legal requirements may vary from state to state and/or change over time. All names have been changed to protect privacy.

Brian Fortenberry is Assistant Vice President of Underwriting at SVMIC where he assists in evaluating risk for the company and assisting policyholders with underwriting issues. He has been involved with medical professional liability insurance since 2007. Prior to his work at SVMIC, Brian worked in the clinical side of medicine and in broadcast media.
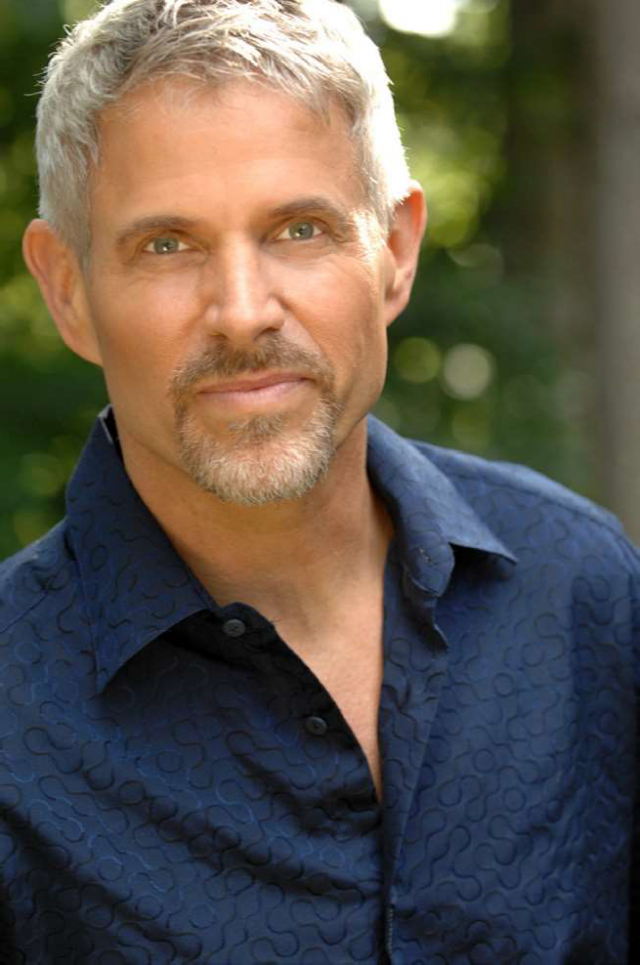
Dr. Dike Drummond is a Mayo trained family doctor, professional coach, author, speaker and trainer whose sole professional focus since 2011 has been addressing the modern burnout epidemic in physicians. He is the CEO and Founder of TheHappyMD.com where he receives 25,000 website visitors a month and hosts an online community of 18,305 physicians from 63 countries around the world. Dr. Drummond has over 2100 hours of one on-one physician coaching experience and has trained over 25,000 doctors on behalf of over 134 corporate clients in the last three years. Dike graduated from the Mayo Medical School in Rochester, Minnesota in 1984 and completed his Family Practice Residency at the Shasta Cascade Program in Redding, California in 1987. Dr. Drummond practiced full spectrum Family Medicine for 11 years as a member of the Skagit Valley Medical Center in Mount Vernon, Washington. He was also the Chairman of the Executive Committee and Managed Care Medical Director for that organization. In 1999, Dr. Drummond left his medical practice due to career ending burnout. He became the COO of Superteams, LLC providing Leadership and Facilitation training to Lean Six Sigma Black Belts in all branches of the US Military. He is a certified Life and Business coach with extensive experience in personal and business development with physicians and entrepreneurs over the last 17 years.